Achondroplasia is the most common form of dwarfism and a well-recognized genetic condition that affects bone growth and development. It is part of a broader group of disorders called skeletal dysplasias, which cause abnormalities in bone size and shape.
Dr. Ahmed Thabet focuses primarily on pediatric patients with achondroplasia, though he also sees adults when appropriate. His care approach combines advanced orthopedic and limb reconstruction techniques with a strong emphasis on improving mobility, comfort, and quality of life in children.

Dr. Ahmed Thabet Hagag sees patients in Angleton, TX and throughout the greater Houston area.
What Is Achondroplasia?
Achondroplasia is caused by a gene mutation in the FGFR3 gene, short for fibroblast growth factor receptor 3. This gene regulates bone growth, particularly at the growth plates, the soft areas of developing cartilage at the ends of long bones in children.
In achondroplasia, the mutation slows down this process, leading to shorter limbs, spinal changes, and characteristic facial features such as a prominent forehead.
This condition occurs in approximately 1 in every 20,000 to 25,000 live births and can be inherited or appear spontaneously without a family history.
Key Characteristics of Achondroplasia
People with achondroplasia typically share distinct physical features. While the condition affects bone growth, cognitive development and overall health are typically within normal limits. Early diagnosis helps monitor growth and prevent complications.
- Disproportionately short arms and legs
- Large head with prominent forehead
- Short stature (average adult height around 4 feet)
- Curved lower spine (lordosis)
- Limited range of motion at the elbows
- Bowing of the legs or spinal curvature
Though achondroplasia is a lifelong condition, many individuals with achondroplasia live full, active lives. Some may face orthopedic challenges that can be improved with specialized care.
Diagnosis and Genetic Testing
Early and accurate diagnosis of achondroplasia allows families to plan for care and monitor for potential complications. There are several ways the condition can be identified:
- Prenatal Diagnosis: In some cases, achondroplasia can be suspected during routine prenatal ultrasounds. Features such as shortened femur length, macrocephaly (enlarged head), or frontal bossing (prominent forehead) may raise concern. If these markers are present, genetic testing through procedures like amniocentesis can confirm the diagnosis by detecting a mutation in the FGFR3 gene.
- Postnatal Diagnosis: After birth, doctors may recognize achondroplasia based on distinct physical features, including a large head with a prominent forehead, shortened limbs, and midface hypoplasia. These findings often prompt further evaluation.
- Genetic Confirmation: A genetic test can confirm the diagnosis by identifying the specific FGFR3 gene mutation responsible. In some cases, imaging such as X-rays may also be used to assess bone development and growth plate characteristics.
Families with a history of achondroplasia may also benefit from genetic counseling to better understand inheritance patterns and reproductive options.
Common Orthopedic Concerns in Achondroplasia
Orthopedic issues are common among individuals with achondroplasia and often emerge during early development. Addressing these concerns proactively can improve comfort, mobility, and overall function.
- Bowed legs and limb deformities that may affect walking
- Narrow spinal canal, which can lead to spinal stenosis or nerve compression
- Knee alignment issues such as bow legs (genu varum)
- Frequent middle ear infection ear infections due to structural differences in the skull
- Slower achievement of motor milestones due to limb proportions
For children with achondroplasia, early evaluation by an orthopedic specialist is key to managing these concerns and planning appropriate treatment when necessary.
Explore our full range of pediatric orthopedic services for children with bone growth or developmental conditions.
Treatment for Achondroplasia
There is no cure for achondroplasia, but many treatments are available to address orthopedic aspects of the condition and improve quality of life. Dr. Thabet provides a full spectrum of care, from observation to complex reconstructive surgery.
Because achondroplasia can affect multiple systems in the body, we take a multidisciplinary approach to care. Dr. Thabet collaborates with pediatricians, ENT specialists, endocrinologists, neurologists, and spine surgeons to ensure each patient receives coordinated, individualized treatment. This team-based model supports both the physical and developmental needs of children with achondroplasia over time.
Learn more about orthopedic surgery options we offer for complex bone and joint conditions.
Non-Surgical Treatments
Non-surgical options often support mobility and help prevent worsening deformities. These treatments are usually considered first, especially in young children.
- Watchful waiting for mild limb differences or deformities that may improve with growth or remain functionally stable.
- Bracing and orthotics to guide growth, including the use of guided growth techniques. Guided growth involves placing small metal plates or screws near the growth plates to gradually correct angular deformities over time. This minimally invasive procedure allows the child’s natural growth to realign the bones without cutting or repositioning them surgically.
- Physical therapy to improve strength, flexibility, coordination, and overall motor development.
- Customized bracing and mobility solutions to support walking, reduce joint strain, and promote independence
In addition to these treatments, new FDA-approved medications such as Voxzogo® (vosoritide) offer promising options for children with achondroplasia. These therapies work by targeting the FGFR3 signaling pathway to promote more normalized bone growth. Vosoritide is administered as a daily injection and is typically considered in partnership with a pediatric endocrinologist for eligible children with open growth plates.
Surgical Options
Surgery may be recommended when significant deformities or functional limitations affect mobility, comfort, or overall quality of life. Each treatment plan is tailored to the patient’s age, growth potential, and long-term goals.
Common surgical procedures include:
- Guided growth to correct angular deformities by placing small plates near the growth plates, allowing gradual realignment during growth.
- Osteotomy to cut and reposition bone for structural realignment.
- Spine decompression surgery to relieve pressure from spinal stenosis or foramen magnum narrowing, when needed.
Limb Lengthening Strategy
Limb lengthening is an elective but highly specialized procedure that may be considered for children with achondroplasia who wish to increase stature or improve limb proportions. Dr. Thabet uses a comprehensive lengthening strategy that includes:
- 4-segment lengthening: Both femurs and tibias are lengthened simultaneously to achieve greater overall height in a more efficient timeline.
- Extended limb lengthening protocol: Typically staged across three separate procedures beginning around age 8–9, with the goal of completing lengthening before high school.
- Arm (humerus) lengthening: Performed after the lower limbs have reached functional goals to improve upper limb reach and balance.
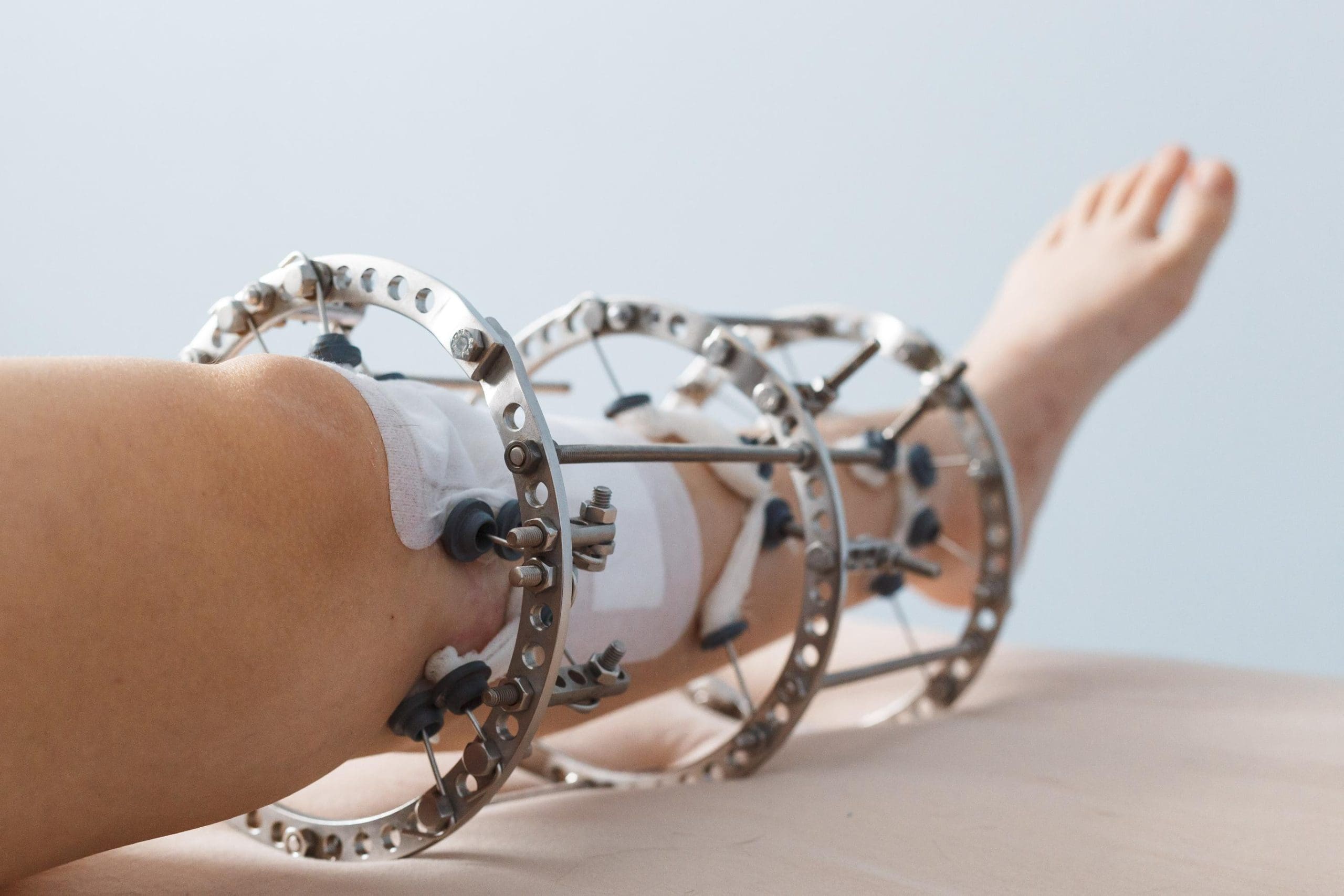
- Devices used: Both external fixators and internal lengthening nails (such as PRECICE) may be used depending on the patient’s anatomy, goals, and recovery considerations.
Limb lengthening is a gradual process, involving two key phases:
- The distraction phase, where the bone segments are slowly separated (about 1 mm per day) to allow new bone to form.
- The consolidation phase, where the new bone hardens and stabilizes over several weeks to months.
Throughout the process, physical therapy and close monitoring are essential to protect surrounding soft tissues, maintain joint mobility, and support long-term success.
Bone and Limb Lengthening for People with Achondroplasia
Bone and limb lengthening is an advanced orthopedic procedure that some people with achondroplasia may consider. It can improve height, balance, and independence.
This process involves gradually growing new bone tissue using an internal or external device. Dr. Thabet uses the latest techniques, including internal magnetic nails, to minimize discomfort and protect surrounding soft tissues. Careful planning helps preserve the growth plates in children and avoid complications.
This treatment is always optional and thoroughly discussed with each patient and family.
Compassionate, Specialized Care
Whether you are seeking early guidance for your child or exploring treatment as an adult, Dr. Thabet provides expert orthopedic care tailored to your goals. From non-surgical management to advanced limb reconstruction, we’re here to support your mobility, comfort, and long-term quality of life.
FAQs
What causes achondroplasia?
Achondroplasia is caused by a gene mutation in the FGFR3 gene, affecting bone growth.
Is achondroplasia always inherited?
While it can be passed down from a parent, most cases result from a new genetic mutation and occur without any family history.
Can you increase height in people with achondroplasia?
Limb lengthening surgery is an option for those seeking increased stature. This involves gradual bone growth using internal or external devices.
What is the lifespan of someone with achondroplasia?
Most people with achondroplasia have a normal life expectancy. With appropriate medical care and monitoring for complications, they can live long, healthy, and active lives.
How prevalent is achondroplasia in the US?
Achondroplasia affects about 1 in every 20,000 to 25,000 live births. It is the most common form of dwarfism and occurs equally across all ethnic backgrounds.
How can I find an achondroplasia specialist near me?
If you’re searching for an orthopedic specialist near you for achondroplasia care, Dr. Thabet welcomes patients from Angleton, Houston, Galveston, League City, and nearby communities across Southeast Texas.