Osteomyelitis is a serious bone infection that can develop after an injury, surgery, or as a complication of chronic health conditions. If not properly diagnosed and treated, it can lead to long-term pain, bone damage, and even limb loss.
The outcome often depends on the balance between the strength of the infection-causing organism (bacteria or fungus) and the body’s immune response. When the immune system is compromised, the risk of severe complications increases.

Dr. Ahmed Thabet Hagag sees patients in Angleton, TX and throughout the greater Houston area.
What Is Osteomyelitis?
Osteomyelitis is an infection in the bone that may present in different forms depending on the severity and duration.
- Acute osteomyelitis: Develops quickly, often with severe pain and systemic symptoms like fever, chills, acute swelling and redness. Requires immediate medical care.
- Chronic osteomyelitis: A persistent or recurring infection that may cause ongoing drainage, pain, or damage to the bone over time.
- Subacute osteomyelitis: Develops more gradually and may not present with typical signs or symptoms.
Infections may spread to the bone from the bloodstream, from nearby soft tissue, or through a direct injury such as a fracture or surgical wound. In people with diabetes, foot ulcers are a common source of infection.
Infection can affect any area of the musculoskeletal system: bone, joints or muscles. The spine is one of the most common areas affected in adults, a condition called vertebral osteomyelitis. Extremities (limbs) are commonly affected too. In children, the infection often settles in the long bones of the legs or arms.
The occurrence of infection in the presence of internal implants is serious and difficult to treat. The bacteria hides around a thin layer of tissues called biofilm. The biofilm prevents the delivery of antibiotics and substances produced by the immune system to fight the infection. That is why these conditions need complex treatment.
Dr. Thabet takes a comprehensive approach to treating bone infections, working closely with a multidisciplinary team that may include an orthopedic surgeon, infectious disease specialist, and other medical doctors to support complete healing.
How It Happens
The infection often starts when bacteria or fungi enter the bloodstream or invade through an open wound. The presence of orthopedics implants adds to the challenges of treatment and eradication of the infection. The biofilm formed around the orthopedics implants prevents the delivery of antibiotics and the immune system.
Once inside the bone, the infection can block blood flow, kill healthy bone (the dead bone is called sequestrum), and spread to nearby tissue. What begins as an isolated issue can turn into a more widespread problem involving infected bone and surrounding structures.
Infection can lead to implant loosening, fixation failure, and ultimately non-healing of the fracture (nonunion). While some infections are obvious, others can go unnoticed. These subtle infections are often caused by weaker organisms that normally live on the skin, in the armpits, or other areas of the body.
Certain patients are at higher risk, including those with diabetes, poor circulation, weakened immune systems, or chronic conditions such as sickle cell disease, rheumatoid arthritis, or cancer. Patients undergoing immunosuppressive therapy or chemotherapy are also more vulnerable.
Getting the Right Diagnosis
Osteomyelitis can be difficult to detect, especially early on. Diagnosis typically involves a combination of:
- A thorough physical examination.
- Blood tests to look for signs of infection and inflammation, including elevated white blood cell counts.
- Blood cultures to identify the specific organism causing the infection-Staphylococcus aureus is one of the most common culprits.
- Blood tests to look for signs of infection and inflammation.
- Imaging such as MRI to assess the bone and surrounding soft tissue.
- Bone scans for early infection.
- Bone biopsy to confirm the diagnosis and identify the type of infection.
- The tissue cultures come back positive 80% of the time. The other 20% can be culture negative.
Treatment Options
Treatment depends on how advanced the infection is. It may be either superficial or deep. A superficial infection affects the tissues above the deep fascia, the thick layer beneath the skin.
In many cases, treatment begins with antibiotics, which are typically effective for superficial infections. This may involve a course of intravenous (IV) antibiotics followed by oral antibiotics until the infection is fully resolved.
Some cases can be managed with IV antibiotics alone, while others, especially deep infection in the presence of deep implants, may require surgery to remove damaged or dead bone and stabilize the area. The decision to remove or swap the implants varies from patient to patient.
Dr. Thabet often collaborates with infectious disease specialists to provide comprehensive care. When surgery is needed, options may include:
- Debridement (removal of infected or dead tissue)
- Retention or implants removal depends on each patient
- Bone grafting or reconstruction
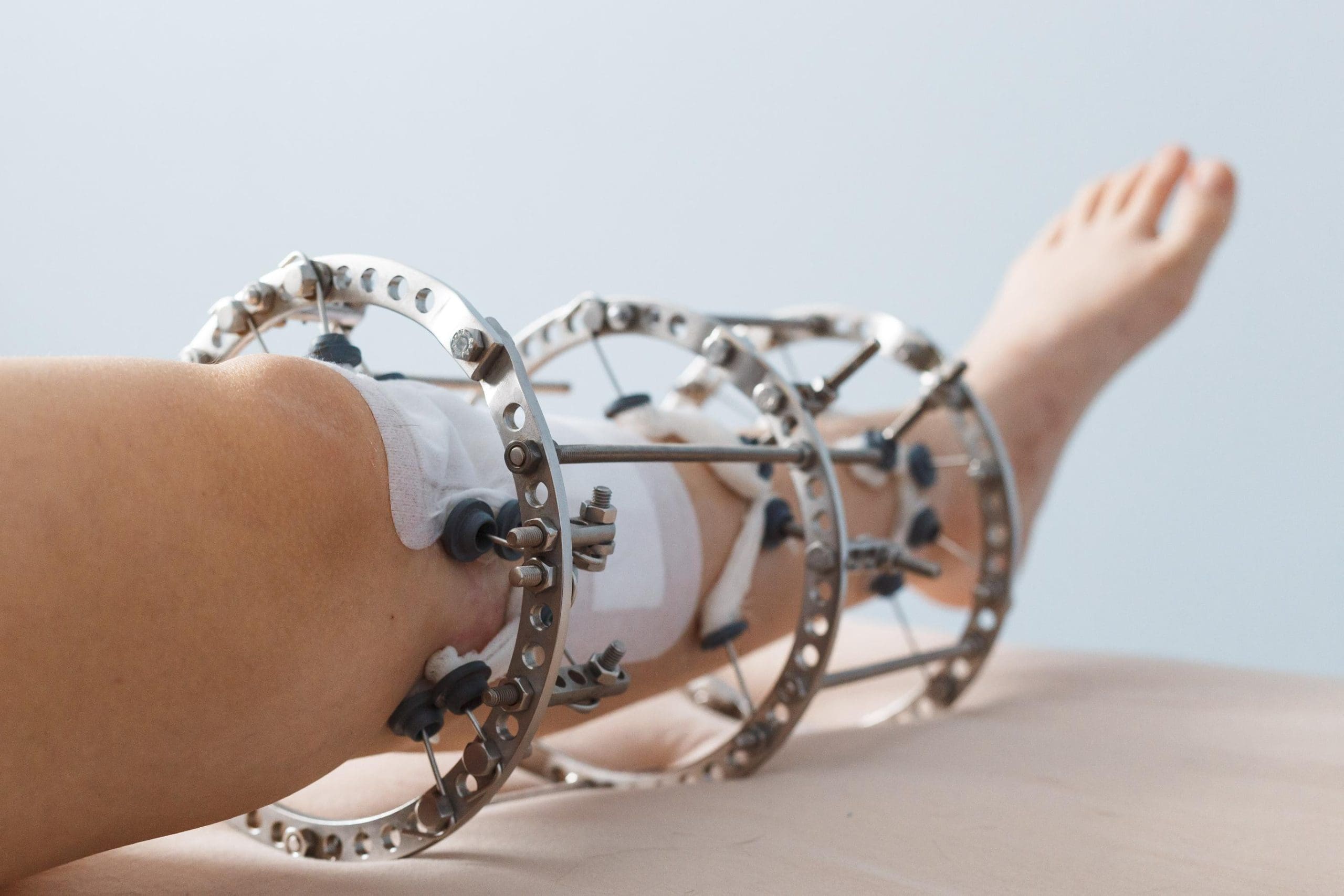
- External fixation to stabilize the bone during healing
- Local antibiotic delivery at the surgical site
- Antibiotics treatment post operatively
Expertise in Complex Bone Infections
Osteomyelitis is one of the more complex conditions we treat. It requires not just infection control, but a plan for preserving mobility and limb function.
Dr. Thabet’s background in orthopedic trauma, limb reconstruction, and bone infection care allows him to offer solutions even in challenging or long-standing cases.
FAQs About Osteomyelitis
What is the cause of osteomyelitis?
Osteomyelitis is most often caused by bacteria that enter the body through the bloodstream, nearby tissue, or direct injury. In cases of acute osteomyelitis, the infection typically spreads rapidly and may develop within days. Chronic osteomyelitis, however, tends to develop over time, often after an injury or surgical complication, and can be more difficult to treat. Risk factors include diabetes, recent surgery, poor circulation, or compromised immunity.
How fast does osteomyelitis spread?
The infection can progress quickly, especially in acute cases. Without treatment, bacteria may destroy bone tissue and spread to nearby soft tissue or joints within days to weeks.
Can osteomyelitis be reversed?
With early diagnosis and appropriate treatment, many cases can be successfully managed. Reversal often requires a combination of antibiotics and, in more severe cases, surgical removal of infected or dead bone.
What are the red flags of osteomyelitis?
Key warning signs include persistent bone pain, swelling or redness over the affected area, drainage from a wound, fever, and fatigue.
What is the difference between chronic osteomyelitis and acute osteomyelitis?
Acute osteomyelitis typically develops quickly, often within days following an injury, surgery, or infection. It usually presents with severe pain, fever, and swelling and is often easier to treat when caught early. Chronic osteomyelitis develops over time and may result from an unresolved acute infection or from long-term issues like poor blood flow or repeated trauma.
How do I find an osteomyelitis specialist near me?
If you’re searching for an orthopedic surgeon near you who treats complex bone infections, Dr. Thabet sees patients in Angleton, TX and welcomes referrals from Houston, Galveston, League City, and surrounding Southeast Texas communities.